Occupational and physical therapists have traditionally been trained from a rehabilitation perspective to treat a wide or diverse range of medical conditions. Many principles of rehabilitation can be applied to various spectrums of chronic health conditions. Conditions such as ME/CFS and Long COVID (LC) require a unique approach both for service delivery methods as well as interventions. While there is a small group of rehabilitation professionals who have basic knowledge of ME/CFS, there is a lack of training and education related to the unique requirements of these medical conditions.
Research, education and treatment protocols related to ME/CFS, and therapy approaches are needed. Therapists are uniquely positioned to start to implement strategies for individuals with ME/CFS and LC that in my opinion can help to improve overall function and quality of life.
I worked as an occupational therapist for almost 30 years and felt that I was very empathetic towards my clients. It wasn’t until I myself developed symptoms and was later diagnosed with ME/CFS, fibromyalgia, MCAS, orthostatic intolerance that I realized that my past knowledge and training was not enough. The debilitating impact of symptoms on everyday function was significant. I tried to apply principles of energy conservation, pacing and adaptation to my daily life.

I realized that with all my training, knowledge and experience, traditional approaches to therapy were not working and a different approach, as well as perspective, was required. I also came to realize from firsthand experience that many health care professionals on my team had limited knowledge of ME/CFS and that resources to help with their education was very limited. I became a teacher to many on my health care team in order to improve basic understanding of my condition.

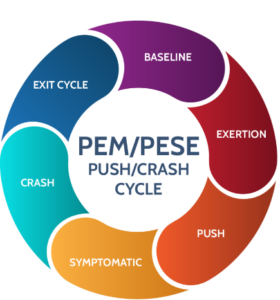
Assessment tools, functional measures and screening tools used by therapists often look at can a person do an activity or not (“yes” or “no”) but does not capture the “cost” to the person completing the task. For example, when I was asked can you dress? Can you shower? Can you walk 25 feet? My answers were “yes”. What the screening did not capture was that it took me almost 2 hours to dress in basic clothing items and that I had to be horizontal on the bed and rest for 10-15 minutes between each item of clothing. I would also then require 30 minutes of complete rest (horizontal on bed, limited stimuli- low lighting, no noise….) before I could walk from my bedroom to living room recliner chair. I was not able to shower and dress within the same 2-hour time span. From a physical strength and ROM perspective, I had the functional abilities to complete the tasks, but the impact of PEM and limited capacity significantly impacted the efficiency of task completion. The cost of completing the simple task of dressing impacted other everyday tasks such as simple meal preparation, reading and having a conversation. Two hours rest in my recliner post dressing was needed before I could do just one of these activities for a short period of time.
As a former occupational therapist as well as educator (college professor for OT/PT assistants) as well as a person with ME/CFS, my desire is to help others with this condition, as well as LC, so that years of suffering may be prevented in the end. It was several years before I started to understand my health condition and what strategies were helpful to improve my overall quality of life and functional status. It took a lot of effort to disseminate information that was helpful and that I could apply to my daily life.
It is my hope that with more and more education of health care professionals, including those who are PT/OT/SLP, about the unique needs and approaches required for ME/CFS and LC that people’s lives will improve and that the harm from “traditional approaches” will be reduced significantly. I wish I had known sooner some strategies that helped to improve my quality of days and decreased impact of symptoms on my everyday living.
Even though I live in Canada, finding the resources of the Bateman Horne Center as well as the monthly support group were a true lifeline to me in the darkest part of my health journey. I have met so many amazing people who share this health condition with me as well as those who have LC.

Thank you for this opportunity. I hope that many people’s lives are impacted by the positive benefits that will be derived from educating health care professionals (and people with ME/CFS and LC themselves).
Sincerely,
Barbara McMaster, BSc (OT), Co-Author of the education series for rehabilitation professionals.

 Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.
Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.