On this page, BHC breaks down the diagnostic criteria for fibromyalgia (FM) and provides videos, handouts, and health management guidance.
What is fibromyalgia?
Fibromyalgia (FM) is a chronic, widespread pain amplification disorder involving both central and peripheral nervous system sensitization throughout the body.
Fibromyalgia is often thought to be a secondary complication of an additional underlying illness or injury that may have promoted these chronic changes in nervous system signaling in a person susceptible to developing the disorder. Fibromyalgia is often accompanied by its own secondary complications including migraines, irritable bowel syndrome, and interstitial cystitis.
Widespread pain, or hyperalgesia, may be described by patients in the following ways:
- Stiffness
- Achiness
- Sharp shooting pain
- Tingling and numbness
- Light and sound sensitivity
- Pain which originates in the muscles, joints, bowel, bladder, pelvis, chest, head
What Causes FM?
The causes of FM remain unclear and may differ from patient to patient. Research suggests involvement of the nervous system, particularly the central nervous system (brain and spinal cord). Fibromyalgia may run in families, and although there is likely a genetic component to the illness, genes alone do not cause FM. There likely are certain genes that can make people more prone to getting fibromyalgia and other comorbid conditions associated with it.
There are often ‘triggering factors’ which sets off FM. Injury, spinal conditions, physical stress, underlying rheumatic conditions, etc. The result is a change in the way the body “talks” with the spinal cord and brain. Levels of brain chemicals and proteins may change. More recently, fibromyalgia has been described as Central Pain Amplification disorder, meaning the volume of pain sensation in the brain is turned up too high.
[Sources: Bateman Horne Center & American College of Rheumatology]
Symptoms
Common manifestations of sensory amplification disorders (FM):
- Muscle and joint pain and tenderness
- Migraine and tension headaches, TMJ/TMD
- Paresthesia (numbness and tingling)
- Restless legs syndrome
- Irritable bowel syndrome, IBS-D, IBS-C
- Irritable bladder, interstitial cystitis, painful menstruation, pelvic pain, vulvodynia
- Sensory (light, noise, olfactory, chemical, etc) sensitivities
- Sicca syndrome (dry eyes and mouth)
- Heart palpitations, sinus tachycardia, low HRV
Research shows nonspecific changes in autonomic nervous system function, dysregulation of the hypothalamic-pituitary adrenal (HPA) axis, and elevation of Substance P, glutamate and other pain neurotransmitters in the cerebrospinal fluid.
Functional MRI scans demonstrate more areas of pain processing in the brain for a given stimulus compared to normal people.
Sleep studies show profound alterations of brain waves during the stages of sleep.
Symptoms can become chronic and very difficult to treat, even after the “stress” is relieved and mood symptoms are well compensated. Poor coping skills or maladaptive behaviors, often related to lack of disease recognition and education, may compound FM symptoms and worsen prognosis.
Diagnosis
2016 revisions to the 2010 FM diagnostic criteria indicate:
An adult meets criteria for being diagnosed with fibromyalgia when all of the following criteria are met:
- Generalized pain, defined as pain in at least 4 of 5 regions, is present.
- Symptoms have been present at a similar level for at least 3 months.
- Widespread pain index (WPI) ≥ 7 and symptom severity scale (SSS) score ≥ 5 OR WPI of 4–6 and SSS score ≥ 9.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
Management
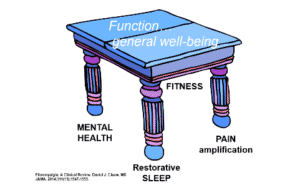
Managing FM often requires a multifaceted approach, which includes the “four table legs” of wellness. Finding a healthy balance between fitness and mental health, while addressing pain and sleep disturbances can greatly improve patient functioning and general well-being.
- Address all chronic or comorbid medical conditions. Dig deeper into any unresponsive or atypical symptoms.
- Prioritize and treat the major illness symptoms but economize medications.
- Incorporate positive behavioral change.
- Use medications that work for more than one aspect of FM (more than one leg of the table).
- Use the lowest effective doses (start low and go slow).
- Avoid causing new symptoms or side effects.
It’s also important to understand and manage the “4 table legs of wellness.”
Pain
- Use medications effective for the type of pain experienced.
- FDA approved for FM: pregabalin, duloxetine, milnacipran.
- Non-FDA approved for FM: gabapentin, amitriptyline, cyclobenzaprine, tramadol, low-dose naltrexone (LDN).
- Non-FM pain may need to be considered and addressed separately (i.e. osteoarthritis).
- Low-Dose Naltrexone (LDN) Management Overview (handout)
- Low-Dose Naltrexone (LDN): A Note to Providers (handout)
Sleep disturbances
- Practice good sleep hygiene.
- Diagnose and treat sleep disorders.
- Utilize appropriate medications, and watch for lingering side effects the following day, as this can lead to more symptoms of “brain fog.”
Psychological state (mental health)
- Strike a balance between your personal and professional demands.
- Practice good self-care and mindfulness exercises.
Deconditioning/Fitness
- Restorative exercise: strength, flexibility, low impact aerobic.
- Be mindful of other comorbid conditions as they impact conditioning and pacing.
- Watch out for ‘Fibro Flares’ caused by overdoing or pushing past your body’s limits.
Education and Management Resources
Educational Handouts & FM-Specific Videos
Other Resources
Educational Handouts
- Low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain
- Helpful hints for treating FM
- Dr. Bateman’s treatment advice to patients
- Fibro Flare FAQ
Videos

 Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.
Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.