What is Myalgic Encephalomyelitis/Chronic Fatigue Syndrome?
Myalgic encephalomyelitis/chronic fatigue syndrome, commonly referred to as ME/CFS, is a disease characterized by profound fatigue, cognitive dysfunction, sleep abnormalities, autonomic manifestations, pain, and other symptoms that are made worse by exertion of any sort (physical, cognitive, emotional, orthostatic stressors).
ME/CFS can severely impair a patients’ ability to conduct their normal lives, yet many struggle with symptoms for years before receiving a diagnosis. It is estimated that ME/CFS affects upwards of 3 million Americans, 80% of which remain undiagnosed, even after years of cycling through specialty care.
What Causes ME/CFS?
The cause of the disease remains unknown, although in many cases, symptoms may have been activated by an infection, virus, or some other triggering event.
The severity of illness ranges from mild to profound in disease presentation. At least one-quarter of ME/CFS patients are house – or – bedbound at some point in their lives. The direct and indirect economic costs of ME/CFS on a societal level, have been estimated between $17—$24 billion annually, including $9.1 billion attributed to lost household and labor force productivity. [Frontiers in Pediatrics]
Diagnostic Criteria
A diagnosis of ME/CFS requires the patient to have three core symptoms:
1. Impairment of normal function accompanied by fatigue persisting > 6 months
2. Post-exertional malaise (PEM)*
3. Unrefreshing Sleep*
Plus at least one of the following manifestations:
4. Cognitive Impairment*
5. Orthostatic Intolerance (OI)
*Must be moderate-severe and present >50% of time
Other common but more variable features of illness include:
- Pain (headache, muscle and joint aches, hyperalgesia/fibromyalgia)
- Immune manifestations (allergy, inflammation, sensitivities)
- Infection (viral or atypical infections)
Understanding the Diagnostic Criteria
Fatigue & Impairment
There is sufficient evidence to suggest that fatigue in ME/CFS is profound, not the result of ongoing excessive exertion, and is not substantially alleviated by rest. This fatigue must be accompanied by a substantial reduction or impairment in one’s ability to engage in pre-illness levels of occupational, educational, social, or personal activities and must persist longer than 6 months.
Fatigue, and particularly the impact of illness on function, should be assessed in making a diagnosis of ME/CFS.
Learn More:
See Activity Intolerance and Cognitive Impairment videos which can be found under the PEM section.
Post Exertional Malaise (PEM)
PEM is the worsening of a patients’ symptoms and function after exposure to physical, cognitive, emotional, or orthostatic stressors that were normally tolerated before disease onset.
PEM is an exacerbation or relapse of symptoms that occurs as a consequence of exertional activity. Exceeding cellular energy capacity results in a “pay back of symptoms” or a “crash” which can occur up to 24-48 hours after peak exertion.
Subjective reports of PEM and prolonged recovery are supported by objective evidence in the scientific literature, including failure to normally reproduce exercise test results (2-day cardiopulmonary exercise test) and impaired cognitive function after exertion.
True PEM appears to be pathognomonic to ME/CFS, and is a distinugishing factor when making a differential diagnosis.
Upright Activity & Exercise Intolerance:
Critical Concepts in the
Evaluation of CFS
Activity Intolerance & Pacing
Management
The most important primary intervention for ME/CFS is activity management (pacing), which includes management of physical, cognitive, emotional, and orthostatic stressors.
Pacing includes:
- Limiting activity to available energy.
- Engage in short activities, which are spread out through the day.
- Engage in recovery behaviors between activities:
- Allow for physical and cognitive rest.
- Recline or lie supine.
- Hydrate.
- Avoid accumulating significant PEM debt.
- Create a self-awareness on when you are accruing PEM debt, and acknowledge that it needs to be paid off as soon as possible. The more debt accrued, the longer it will take to pay off the ‘energy debt.’
“Pacing” reduces the frequency and severity of PEM and improves both symptoms and function.
- Ideally, engage only in the amount of activity that doesn’t induce PEM in 24-48 hours.
- The goal of pacing is to feel “back to baseline” the following morning after a night of restorative sleep.
- If PEM is induced, it is crucial that you rest until it resolves.
- Try not to ruminate on the crash, but rather set aside time for body/energy check-ins and structured rest time moving forward.
- Develop a heightened sense of awareness about the threshold of relapse, and the consequences of pushing beyond it.
Activity logs, heart rate monitors, smart watches, and the Oura Ring are all helpful tools to give immediate/daily/weekly/monthly feedback on activity and pacing.
Unrefreshing Sleep
Sleep that remains non-restorative regardless of sleep duration, is a key factor when identifying the presence of this symptom. Polysomography often shows abnormal sleep architecture in those with ME/CFS, which includes: delayed onset of sleep, fragmented sleep, increased alpha waves (light sleep) and decreased delta waves (deep sleep). Although polysomnography is not required to make a diagnosis of ME/CFS, it may be useful to identify or rule out the presence of a manageable sleeping disorder (ie: sleep apnea, insomnia, etc.).
Management
Management
- Practice good sleep hygiene (keep a routine, calm/cool environment)
- Rule out primary sleep disorders. If identified, treat.
- Minimize sedating medications during the day time.
- Avoid caffeine, alcohol, decongestants, and/or stimulants before bed.
- Avoid brain activating activities before bed.
- Address central sensitivities which may be disturbing sleep (ie: restless leg syndrome, pain amplification, central ‘overload’ (PEM).
- Sleep monitoring devices can provide valuable feedback on sleep quality and episodes of wakefulness.
- Plan your day accordingly. If you had minimal restorative sleep the night before, schedule more structured rest periods throughout your day to avoid slipping into energy debt (PEM).
Cognitive Impairment
Impairments of cognitive function, and particularly slowed information processing are frequently reported in those with ME/CFS. Cognitive performance often worsens as a consequence of continued physical, mental, emotional, and/or orthostatic exertion. Symptoms can wax and wane with energy expenditure.
Patients often report problems with short term memory, concentration, and difficulty multi-tasking. Cognitive slowing, cognitive fatigability, and cognitive PEM may be the most limiting aspects of ME/CFS and is a primary reason many are unable to sustain employment or school.
Management
- Address other co-morbid conditions that could be compounding cognitive impairment (ie: anemia, thyroid, diabetes, sleep apnea, low Vitamin B12, etc.).
- Address the major aspects of illness:
- Pain: reduce severe pain
- Sleep: achieve restorative sleep
- Mental wellness: address any secondary mental health conditions; practice mindfulness, meditation, brain-breaks
- Fitness: engage in restorative exercise-within reason! Avoid slipping into energy debt (PEM). Start low, go slow.
- Pace to prevent symptom escalation:
- Preventative activity management
- Reduce overload (avoid PEM)
- Address potential contributors to ‘brain fog’ (ie: medications, sleep dysfunction, low cellular energy production, OI, etc.).
Orthostatic Intolerance
Orthostatic Intolerance (OI), Orthostatic Hypotension (OH), Neurally Mediated Hypotension (NMH), and Postural Orthostatic Tachycardia Syndrome (POTS) are terms used to describe the exacerbation of symptoms during upright posture, that are relieved or ameliorated by lying down or reclining.
Symptoms of OI may present as lightheadedness, headache, fatigue, tremors, heart palpitations, exercise intolerance, nausea, sensitivity to heat, and sleep abnormalities. Patients may describe difficulty with cognitive processing (word finding, concentration, forming sentences).
While the phenomenon is complex and not fully understood, the usual signals or mechanisms that maintain blood vessel tone, heart rate and contractility while changing positions from lying to standing don’t work correctly. This leads to venous pooling, decreased blood return to the heart, and lower cardiac output to the brain and body. Some people are aware of symptoms that occur during the episode, such as dizziness or palpitations (a sensation of increasing heart rate or intensity of each heart beat), while others are not. The body compensates in varied ways for these changes. On occasion, the person actually faints. Others develop rapid heart rate (tachycardia). NMH, POTS, OH are common manifestations of OI in ME/CFS and Fibromyalgia Syndrome (FM).
Management
Recognize and avoid common triggers:
- Heat- avoid becoming over heated
- Dehydration
- Prolonged standing in place
- Prolonged sitting
- Prolonged bedrest (confuses the ANS)
- Muscle atrophy and weakness in the abdomen/core and legs
- Medications that cause/worsen OI
Interventions for OI:
- External compression
- Compression socks, pants, sleeves, abdominal binder
- Key: the more surface area covered, the more compression of blood back to your core
- Internal constriction (ie: pharmacological interventions)
- Increase volume in the vasculature (blood vessels)
- Consume extra water/fluids to expand blood volume
- >1 gallon or >2 liters daily as a foundation
- Increased salt intake helps retain water in the circulation and tissues
- Must match the fluid intake. 2-5 gms daily (1/2 to 1 tsp)
- Rapid water ingestion- (16oz) helps reduce OI within 20 minutes (chugging)
- Pharmacological interventions to increase blood volume. Control/cap the rapid heart rate response (if advised).
- Pharmacological interventions (beta blockers-monitor use!)
Management Resources
Common Food Items High in Sodium
Orthostatic Intolerance Educational Handout
10-Minute NASA Lean Test (Patient Instructions)
10-Minute NASA Lean Test (Provider Instructions)
Important and Frequently Reported Symptoms
that Support Diagnosis:
Immune impairment: Acute infection-like onset, susceptibility to infection, perpetual flu-like symptoms, sore throat, tender lymph nodes, fever, new or worsened sensitivities to certain substances (e.g. foods, odors, medications, chemicals). Poor NK cell cytotoxicity (NK cell function, not number) correlates with illness severity in patients and could serve as a biomarker for the severity of the disease.
Neurological impairment: Impaired psychomotor function, muscle weakness, twitching, instability, spatial disorientation, ataxia, sensory changes (e.g. sensitivity or intolerance to light, noise and touch).
Pain: Headaches, arthralgia, myalgia, other pain symptoms (all highly variable in presence, nature and severity).
- To learn more on amplified pain syndromes, please see our Fibromyalgia page, and the Chronic Fatigue and Pain series located on the medical provider page.
Other: Gastrointestinal impairments, genitourinary impairment, neuroendocrine manifestations (e.g. cold extremities, weight change, excessive sweating, high/low temperature, chills/shivers, loss of appetite, alcohol intolerance).
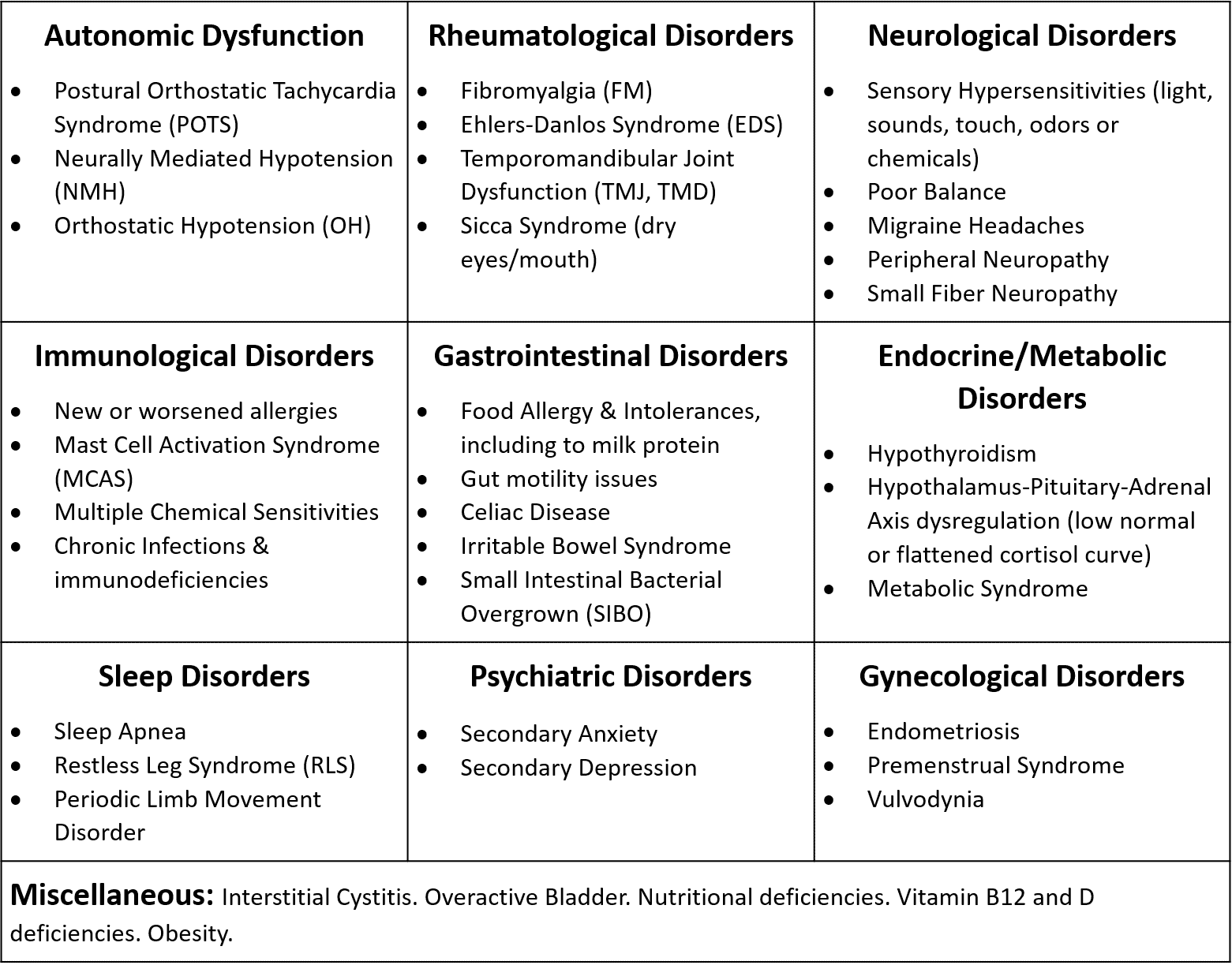
Common Comorbid Conditions
*Content is the property of the U.S. ME/CFS Clinician Coalition.
The following reflects the 2020 U.S. ME/CFS Clinician Coalition’s Guidelines: Basics of Diagnosis and Treatment.
In the past, a diagnosis of ME/CFS was made by first excluding all other possible conditions. However, the 2015 National Academy of Medicine report established ME/CFS as a positive diagnosis that can coexist with other conditions, including those in the differential diagnosis. Recognizing comorbid conditions early, and treating them appropriately, may improve the patient’s health, function, and quality of life.
ME/CFS in Children and Adolescents
ME/CFS is often thought of as an adult disease, but children (both adolescents and younger children) are diagnosed with ME/CFS.
Not as much is known about ME/CFS in children because there have been few studies in this age group. Scientists estimate that up to 2 in 100 children suffer from ME/CFS. This disease is more common in adolescents than in younger children.
- Symptoms & Diagnosis (CDC)
- Treatment of ME/CFS in Children (CDC)
- Pediatric ME/CFS (IOM)
- ME/CFS in Children Fact Sheets
Other Helpful Resources
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer -Frontiers in Pediatrics
Children and Young Adults with ME/CFS – Solve ME/CFS Initiative
ME/CFS in Adolescents– American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society
Interested in research for/about ME/CFS
- Research at BHC: *Please see BHC’s research page to learn more on current and past studies
- Learn about ongoing research:
 Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.
Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.