Bateman Horne Center conducted a research study assessing hemodynamic changes in people with ME/CFS using the 10-Minute NASA Lean Test in 2018/2019. This study culminated in the scientific paper “Hemodynamics during the 10-minute NASA Lean Test: evidence of circulatory decompensation in a subset of ME/CFS patients,” published in the Journal of Translational Medicine.
This study culminated in the scientific paper “Hemodynamics during the 10-minute NASA Lean Test: evidence of circulatory decompensation in a subset of ME/CFS patients,” published in the Journal of Translational Medicine.
There is an interesting story behind the 10-Minute NASA Lean Test. As part the CDC multisite study of ME/CFS [Multi-site clinical assessment of myalgic encephalomyelitis/chronic fatigue syndrome /MCAM] (1) all clinical sites began using the 10-Minute NASA Lean Test (NLT), a clinical tool shared with the group by Dr. Benjamin Natelson and included in the protocol. Once we began enrolling research patients, I realized – and was actually a bit horrified to realize – the NLT was a far superior “bedside” test to assess the impact of orthostatic stress. Much better than the way I was taught to do orthostatic testing as a general internist and had been doing for 20 years. I was horrified because I wondered how many times in 20 years I had completely missed an important diagnosis and treatment option for my patients.
 The most important differences distinguishing the NLT from older methods were establishing relaxed, baseline supine values of heart rate and blood pressure, then leaning against the wall instead of standing to reduce influence of the “muscle pump” in the lower extremities, and then extending the test the full 10 minutes. I also became aware of how many factors influence the test results, such as fasting, pain, anxiety, fluid and sodium intake, medications, wearing compression socks, etc.
The most important differences distinguishing the NLT from older methods were establishing relaxed, baseline supine values of heart rate and blood pressure, then leaning against the wall instead of standing to reduce influence of the “muscle pump” in the lower extremities, and then extending the test the full 10 minutes. I also became aware of how many factors influence the test results, such as fasting, pain, anxiety, fluid and sodium intake, medications, wearing compression socks, etc.
We soon began using the NLT regularly in the clinic as a clinical assessment for all new patients, and as a tool for monitoring treatment in existing patients. The results were energizing. Most ME/CFS patients had meaningful findings and participation in the NLT test made them very ill. Some fainted and some developed tonic-clonic movements, which is a seizure-like response to fainting. Many of these patients had been previously labeled as malingering or given the diagnosis of “pseudoseizures,” which many doctors consider a psychiatric conversion disorder. Most importantly, treating the orthostatic intolerance was helpful for reducing symptoms and improving function in many patients with ME/CFS. We tried to understand what it was telling us.
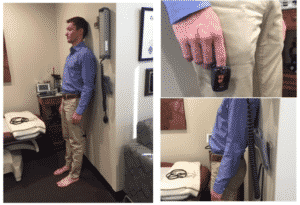 With the help of pre-med student, Pelle Wall (our model in the adjacent photo), and seed funding from the Hutchins Foundation, we conducted a pilot study subjecting 25 ME/CFS patients and 25 healthy controls (HC) to the NLT. Enthusiastic about our hypothesis, we included the NLT in our NIH funded collaboration as the clinical core with the Jackson Laboratories, and later as the clinical project with Columbia University’s Center for Solutions.
With the help of pre-med student, Pelle Wall (our model in the adjacent photo), and seed funding from the Hutchins Foundation, we conducted a pilot study subjecting 25 ME/CFS patients and 25 healthy controls (HC) to the NLT. Enthusiastic about our hypothesis, we included the NLT in our NIH funded collaboration as the clinical core with the Jackson Laboratories, and later as the clinical project with Columbia University’s Center for Solutions.
An initial and confusing finding was that many HC also had an abnormal response to the NLT, which is definitely a significant orthostatic challenge. We dug further into the data, hoping to explain our clinical observation that ME/CFS patients do not tolerate or recover from the NLT as well as HC, regardless of whether criteria for a diagnosis of POTS, orthostatic hypotension or NMH were met. What we learned is that people with ME/CFS, regardless of the BP, HR and PP results, suffer consequences of upright-ness.
Our results were consistent with the work of David M Systrom (2) and bolstered by two publications from van Campen et al in 2020, showing that cerebral blood flow is diminished in ME/CFS during Tilt Table testing, even in the absence of hypotension or tachycardia (3), and that this orthostatic stress causes measurable cognitive impairment (4). We have unpublished data to replicate the latter.
We hope this paper creates an interest in using the NLT as an objective clinical tool that can lead to supportive treatments, but also that it will stimulate interest within the scientific community to explain the physiological underpinnings of these findings. Read the paper here!
—————————————-
1) Multi-Site Clinical Assessment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (MCAM): Design and Implementation of a Prospective/Retrospective Rolling Cohort Study Unger ER, Lin JS, Tian H, Natelson BH, Lange G, Vu D, Blate M, Klimas NG, Balbin EG, Bateman L, Allen A, Lapp CW, Springs W, Kogelnik AM, Phan CC, Danver J, Podell RN, Fitzpatrick T, Peterson DL, Gottschalk CG, Rajeevan MS; MCAM Study Group. Am J Epidemiol. 2017 Apr 15;185(8):617-626. doi: 10.1093/aje/kwx029.
2) Unexplained exertional dyspnea caused by low ventricular filling pressures: results from clinical invasive cardiopulmonary exercise testing. William M. Oldham,1,2,3 Gregory D. Lewis,3,4 Alexander R. Opotowsky,2,3,5 Aaron B. Waxman,1,2,3 David M. Systrom1,2,3. Pulm Circ 2016;6(1):55-62. DOI: 10.1086/685054.
3) Cerebral blood flow is reduced in ME/CFS during head-up tilt testing even in the absence of hypotension or tachycardia: a quantitative, controlled study using doppler echography. van Campen, C. L. M. C., Verheugt, F. W. A., Rowe, P. C., and Visser, F. C. (2020). .Clin. Neurophysiol. Pract. 5, 50–58. doi: 10.1016/j. cnp.2020.01.003
4) Cognitive Function Declines Following Orthostatic Stress in Adults With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). C. (Linda) M. C. van Campen1*, Peter C. Rowe2, Freek W. A. Verheugt3 and Frans C. Visser1 Frontiers in Neuroscience. published: 26 June 2020. doi: 10.3389/fnins.2020.00688
 Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.
Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.