I’ve fought since 2001 to increase awareness in the medical community about ME/CFS, fibromyalgia, and related illnesses. In 2015 we strategically formed the Bateman Horne Center, using a unique non-profit model to promote research, clinical care, and provider education. Linda Tannenbaum and OMF have a parallel story but are more closely aligned to research progress. Then, as has become increasingly evident, the COVID-19 pandemic pushed viral infection, immunity, inflammation, and now post-viral syndromes into the urgent consciousness of medical, scientific, and public institutions. There is no more important time to provide strong leadership, in both education and research based on decades of experience, to this pressing worldwide situation.
Within the last 15-20 years, we have learned about conditions like, or comorbid with, ME/CFS, FM, and related illnesses, such as mast cell activation syndrome (MCAS), syndromes of orthostatic intolerance (OI), small fiber polyneuropathy (SFPN), hypermobile Ehler’s Danlos syndrome (hEDS), and others. We want to teach clinical providers to identify and manage these comorbid conditions, along with long COVID, which can lead to significant improvements in functional capacity and quality of life.
To accomplish these lofty goals, both non-profit organizations (BHC and OMF) will need ongoing financial support. Medical insurance and membership fees do not cover the services BHC provides to patients, which include detailed and individualized care in clinic, educational materials, and ongoing support groups for the broader community. Research in this field is notoriously underfunded. Funds for training clinical providers are virtually unheard of in our field. Thank you for your generous donations in the past and please continue if you can.
Those of you who are my patients, I encourage you to review your options to see other BHC providers if helpful or bond with your PCP and associated medical team, and educate them about this illness complex. Honestly, we will only make progress for others in the future if we come out of our silos and infiltrate the rest of medicine!
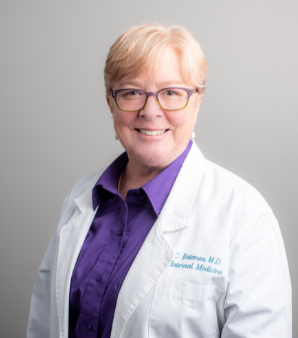
 Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.
Lucinda Bateman, MD, is a renowned clinician, researcher, and educator. Her Johns Hopkins University Medical School training instilled an approach to care that she has employed throughout her career - the patient comes first and the unknown or unexplained does not equate to a lack of proper and compassionate care. Since starting her own practice in 2000, she has served on six boards or committees, been the principal investigator for 45 studies, authored/coauthored 40 journal articles, served as adjunct instructor and adjunct assistant professor in the University of Utah Departments of Preventative Medicine, Internal Medicine, and Anesthesiology, and lectured around the world.